Peter Attia, MD, is convinced that human health is determined by how long one can delay chronic disease onset.
This post will explore Peter’s top 5 most important blood tests, as per his AMA #14.
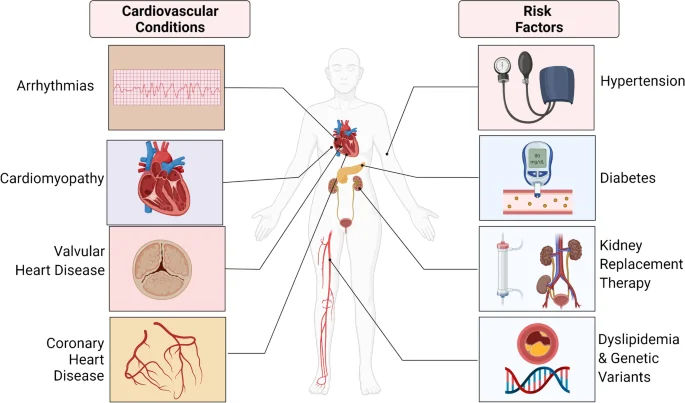
The Four Horsemen of Chronic Disease
The earlier an individual learns what is in their blood and takes action on it, the higher their chances for delaying or avoiding a chronic illness.
In Peter’s opinion, the Four Horsemen of chronic disease are:
- Heart Disease
- Cancer
- Neurodegenerative diseases (such Alzheimer’s disease)
- Type 2 diabetes and related metabolic dysfunction.
Whilst in practice diabetes only ranks as #7 or #8 in terms of the leading causes of death in the USA, Peter believes the impact of metabolic dysfunction, which eventually presents as diabetes, is much higher.
He posits that patients with metabolic dysfunction face a greater risk of the other 3 horseman, compared to those without it (discussed in chapter 6 of his book Outlive).
With this context in mind, we can better understand the value of screening for metabolic dysfunction via blood tests. Detecting issues early gives us more time to correct them before they manifest in disease.

Peter Attia’s Top 5 Most Important Blood Tests
Next we’ll look at Peter’s top 5 tests. This is how they correlate with the four chronic diseases we looked at earlier:
- Tests 1 + 2 look primarily at heart disease risks
- Test 3 + 4 look primarily at metabolic dysfunction
- Test 5 looks at genetic risk related to Alzheimer’s disease
Test 1: Lipoprotein (a) (Lp(a)-P) Test
Lipoprotein Lp(a) is a combination of fat and protein that transfers cholesterol in the blood.
Based on the cholesterol hypothesis, which Peter Attia subscribes to, elevated levels of these substances threaten arteries’ health and signal metabolic issues.
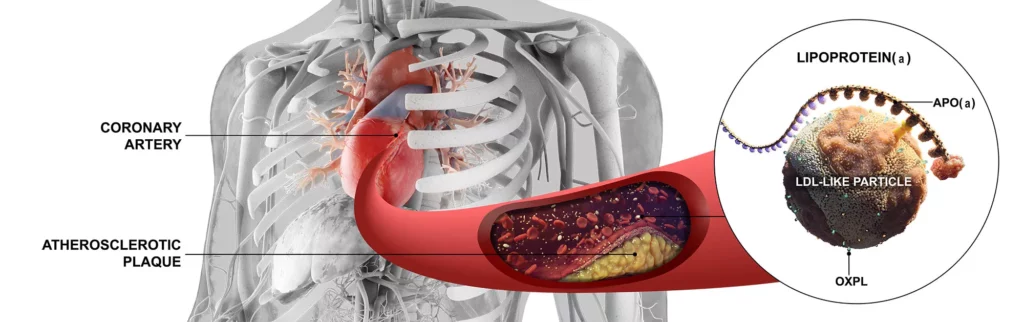
According to the cholesterol hypothesis, the Lipoprotein (a) test, known as Lp(a)-P, is a useful blood screening tool for diagnosing heart conditions and evaluating the risk of developing vascular diseases. Atherosclerosis is one of the most common of these diseases and is considered by Peter as a major pillar of chronic illnesses.
The Lp(a)-P test may be particularly important for individuals with:
- Past heart disease
- High LDL cholesterol levels
- Family history of cardiovascular issues
The Lp(a)-P test is a regular vein blood draw performed in a lab, hospital, or at-home conditions. A patient should fast for more accurate measurements 8-12 hours before the procedure.
The optimal range of Lp(a), according to the National Institutes of Health (NIH), is <14mg/dL1Lipoprotein A – Khashayar Farzam and S. Senthilkumaran | 2022 | StatPearls.
| Optimal | Borderline Risk | High Risk |
| <14mg/dL | 14-30mg/dL | 31-50mg/dl |
Peter recommends finding a lab that provides clients with an Lp(a) measurement in nanomoles per liter (nmol/L) for better risk estimation.
Lipoprotein (a) remains relatively stable and does not require frequent measurements. However, in AMA #14, Peter reminds us that the earlier an individual knows their risk of atherosclerosis, the more effective action they take to delay the chronic disease.
For instance, supplements with l-carnitine, coenzyme Q 10, and Xuezhikang (XZK) appear to have a long-term Lp(a) decreasing effect, as per recent studies2Dietary Natural Products as Emerging Lipoprotein(a)-Lowering Agents – Amir Abbas Momtazi-Borojeni et al. | 2019 | Journal of Cellular Physiology.
Test 2: LDL-P (or ApoB) Test
According to the cholesterol hypothesis, low-density lipoprotein particles (LDL-P) are the unhealthy cholesterol that forms plaques in arteries.
Apolipoprotein B (ApoB) transmits LDL-Ps between organs, and its levels increase with the particles’ volume in the blood.

Doctors assign the LDL-P and ApoB tests when the standard lipid panel fails to provide precise cardiovascular disease risk evaluation or when the results are inconsistent with symptoms.
In his post about measuring cardiovascular disease risks, Peter notes that even if one’s standard lipid panel results are within the norm, LDL-P test results may be high, signaling a higher risk of cardiovascular disease.
Both LDL-P and ApoB tests are simple blood draws that do not require fasting and are performed in laboratories offering lipid panels.
The optimal ranges of these substances in one’s blood are:
- ApoB (mg/dL) <65
- LDL-P (nmol/L) <1000
The levels of ApoB above 110 mg/dL or LDL-P above 2000 (nmol/L) signal the highest risk and require urgent intervention.
Individuals with high LDL-P or ApoB levels can regulate the levels mainly by changing their diet. The Oxford study shows that adding Omega-3-rich products or supplements is also helpful3Dietary, Macronutrient, Micronutrient, and Nutrigenetic Factors Impacting Cardiovascular Risk Markers Apolipoprotein B and Apolipoprotein A1: A Narrative Review – Gregory S Nacarelli et al. | 2023 | Nutrition Reviews.
Peter avoids transfats and consumes vegetables and other fiber-rich products without limits to keep harmful cholesterol levels low. Check our post, Peter Attia Diet – What He Eats & Why, for more information about his nutrition.
Test 3: Oral Glucose Tolerance Test (OGTT)
OGTT measures bodily response to insulin, and in AMA #51, Peter calls it one of the most critical metrics for assessing metabolic health.
The test demonstrates how sugar is being absorbed by cells, and abnormal results signal severe metabolic changes that increase the risks of developing diabetes and cardiovascular disease.
OGTT is a comprehensive procedure; a patient should fast for 8-12 hours before it. In the laboratory, the following happens:
- A blood sample is drawn as a baseline.
- The client drinks glucola, a glucose-only substance, and sits still during the entire test.
- For the next 2 hours, blood is drawn every 30 minutes, and insulin is measured in each sample.
Peter’s description of OGTT ranges in AMA #51 indicates that blood glucose levels above 200 mg/dL at the two-hour mark are suggestive of diabetes.

If the insulin measurements are in the risk zone, lifestyle changes can take place to improve metabolic processes.
Reducing carbohydrates is one of the most effective tactics for decreasing insulin resistance4Effect of Low-Carbohydrate Diets on Cardiometabolic Risk, Insulin Resistance, and Metabolic Syndrome – Blair J. O’Neill | 2020 | Current Opinion in Endocrinology & Diabetes and Obesity. Regular exercise is proven to be one of the most effective tactics for better insulin proceeding5A Comparison of the Impact of Exercise Training With Dietary Intervention Versus Dietary Intervention Alone on Insulin Resistance and Glucose Regulation in Individual With Overweight or Obesity: A Systemic Review and Meta-Analysis – Mousa Khalafi et al. | 2022 | Critical Reviews in Food Science and Nutrition. Peter has optimal physical activity protocols available in this post.
Test 4: The ALT Test
Alanine transaminase (ALT) is an enzyme in one’s liver – the powerhouse of human metabolism. The ALT test assesses liver health because if the organ is damaged, ALT leaks into the blood. The high level of ALT in one’s blood signals the liver cells’ injury.
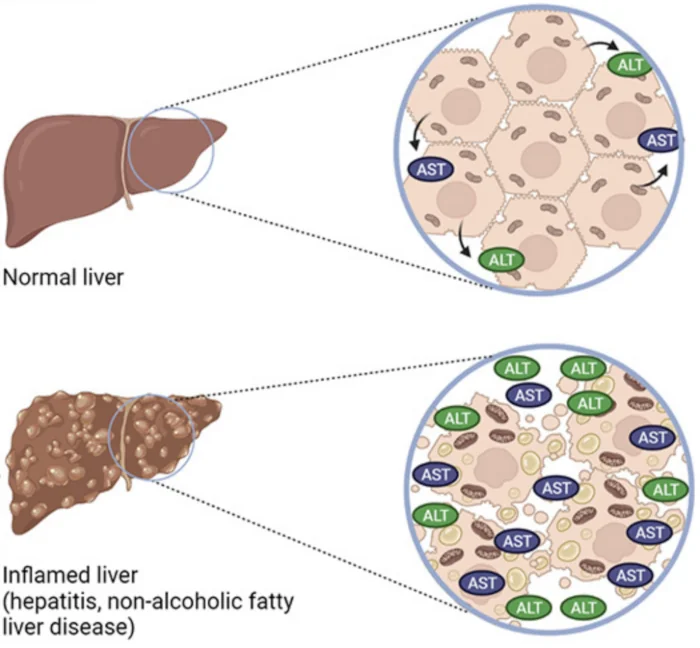
In the podcast episode with researcher Rob Lustig, Peter says that ALT increases when one’s liver stores fat, identifying a metabolic problem.
Individuals with these factors should consider taking an ALT blood test urgently:
- Extensive alcohol consumption
- Family history of liver or metabolic issues
- Obesity
- Diabetes
Standard hospitals and labs include ALT in the liver panel, but some offer ALT-only bloodwork. The panel requires 10-12 hours of fasting, yet the separate ALT blood draw is done without preparation.
Most laboratories count the 7 to 55 U/L as the normal result for the ALT blood test.
In his book Outlive: The Science and Art of Longevity, Peter emphasizes that when it comes to liver health, “normal” is not the same as “healthy” and offers even lower ranges to indicate a risk of liver disease earlier:
- <25 U/L optimal for males
- <20 U/L optimal for females6Outlive: The Science and Art of Longevity – Peter Attia with Bill Gifford | 2023 | Harmony
Regulating and lowering ALT levels in the blood requires improving liver health, mainly with dietary changes. Research marks the following products beneficial for one’s liver:
- Food or supplements rich in Vitamin B9 (dark green vegetables, beans, whole grains)
- Food or supplements rich in Vitamin E (peanuts, avocados, pumpkin)7The Role of Vitamins in Non-Alcoholic Fatty Liver Disease: A Systematic Review – Rose Anne M. Abe et al. | 2021 | Cureus
- Coffee8Coffee as Chemoprotectant in Fatty Liver Disease: Caffeine-Dependent and Caffeine-Independent Effects – Jonathan A. Dranoff | 2023 | Gastrointestinal and Liver Physiology

Test 5: APOE Genotype
APOE is a protein that participates in lipid metabolism, and its gene contains 3 (ε4, ε3, and ε2) alleles carrying the risk of predisposition for Alzheimer’s (AD) and cardiovascular disease.
In the Drive podcast episode #147, Peter and physician Hussein Yassine describe APOE as the conductor of the peripheral circulation system, involved in lipoproteins distribution and metabolism.

Peter included the APOE Genotype in his top blood tests because it determines the combination of alleles and allows one to evaluate their risks of developing chronic diseases.
The APOE genotype is prescribed for adults with dementia symptoms, such as:
- Loss of memory, struggling to remember recent events
- Getting lost in familiar locations
- Family history of multiple relatives with severe Alzheimer’s disease
Human genotype is permanent, so the APOE analysis is a one-time procedure with lifelong relevant results.
Genotyping is a simple blood draw that does not require preparation. The results interpret the risks of AD development based on the alleles found.
| Genotype | e2/e2 | e2/e3 | e2/e4 | e3/e3 | e3/e4 | e4/e4 |
| Risk | 40% less likely | 40% less likely | 2.6 times more likely | Average risk | 2.3 times more likely | 14.9 times more likely |
APOE genotyping is comprehensive, and only specific laboratories offer it. One can contact these labs directly or request a prescription from their healthcare providers.
If one does come back with an APOE4 diagnosis, this provides the opportunity to be pragmatic. Various sources of information for APOE4 exist online, including the APOE4 forums, which have comprehensive resources for prevention strategies.
Roundup
In this post we’ve shone a light on Peter’s Top 5 blood tests.
However, in practice when working with patients, Peter would test a lot more biomarkers.
For more on what Peter has to say, follow his podcast, and/or subscribe to his Premium member’s service.
If you’ve questions on the article, please leave them in the comment section below.
Further Reading
If you found this post interesting, you may also like:
- Peter Attia’s Diet – What He Eats & Why
- Peter Attia Exercise Routines – How He Trains & Why
- Peter Attia’s Supplements – What He Takes & Why
References
- 1Lipoprotein A – Khashayar Farzam and S. Senthilkumaran | 2022 | StatPearls
- 2Dietary Natural Products as Emerging Lipoprotein(a)-Lowering Agents – Amir Abbas Momtazi-Borojeni et al. | 2019 | Journal of Cellular Physiology
- 3Dietary, Macronutrient, Micronutrient, and Nutrigenetic Factors Impacting Cardiovascular Risk Markers Apolipoprotein B and Apolipoprotein A1: A Narrative Review – Gregory S Nacarelli et al. | 2023 | Nutrition Reviews
- 4Effect of Low-Carbohydrate Diets on Cardiometabolic Risk, Insulin Resistance, and Metabolic Syndrome – Blair J. O’Neill | 2020 | Current Opinion in Endocrinology & Diabetes and Obesity
- 5A Comparison of the Impact of Exercise Training With Dietary Intervention Versus Dietary Intervention Alone on Insulin Resistance and Glucose Regulation in Individual With Overweight or Obesity: A Systemic Review and Meta-Analysis – Mousa Khalafi et al. | 2022 | Critical Reviews in Food Science and Nutrition
- 6Outlive: The Science and Art of Longevity – Peter Attia with Bill Gifford | 2023 | Harmony
- 7The Role of Vitamins in Non-Alcoholic Fatty Liver Disease: A Systematic Review – Rose Anne M. Abe et al. | 2021 | Cureus
- 8Coffee as Chemoprotectant in Fatty Liver Disease: Caffeine-Dependent and Caffeine-Independent Effects – Jonathan A. Dranoff | 2023 | Gastrointestinal and Liver Physiology
Disclaimer: The above information is for research and educational purposes only and not a substitute for professional medical advice. See full medical disclaimer.